Certain media reports about Acadia Healthcare paint a false picture of our policies, practices, and standards of care at our hospitals. Not only do these stories misrepresent the facts, but they also omit material context and ignore Acadia’s proven track record of delivering life-saving care to over 150,000 patients facing severe mental health crises in our acute hospitals last year.
To be clear: we patently reject claims that Acadia places profits over patients – including inferences that we systematically hold patients longer than is medically necessary for financial reasons.
Here are some important facts you should know:
- Patient care decisions, including whether treatment is necessary and for how long, are medical decisions made by licensed providers, based on medical necessity and adhere to all associated legal requirements.
- The average length of stay at Acadia’s acute hospitals is in line with national averages.
- In most cases, the decision to involuntarily commit a patient for psychiatric evaluation in a behavioral health hospital is initiated by emergency room providers, law enforcement personnel, or other individuals as designated by state statutes. Those independent third parties make the initial determination that a patient requires hospitalization and evaluation.
- Our hospitals are highly regulated and are required to meet policies and standards set by federal, state, and local governments. Acadia’s acute care hospitals have been inspected and surveyed by The Joint Commission (TJC), the Centers for Medicare & Medicaid Services (CMS) and various state agencies nearly 300 times per year on average over the past five years.
- It is widely recognized within the medical community that discharging patients too early can result in catastrophic consequences, including serious injury – and even death – for the patient or others. Determining the appropriate level of care for acutely ill patients is a complicated and highly individualized decision that psychiatrists across the industry face every day.
Acadia follows industry-standard, clinically driven admission and discharge criteria
To reiterate: we patently reject claims that Acadia places profits over patients – including inferences that we systematically hold patients longer than is medically necessary for financial reasons. Notably, the average length of stay at our acute hospitals is in line with national averages.
Average Length of Stay in Days: Acadia Acute Hospitals vs Industry*, FY2023
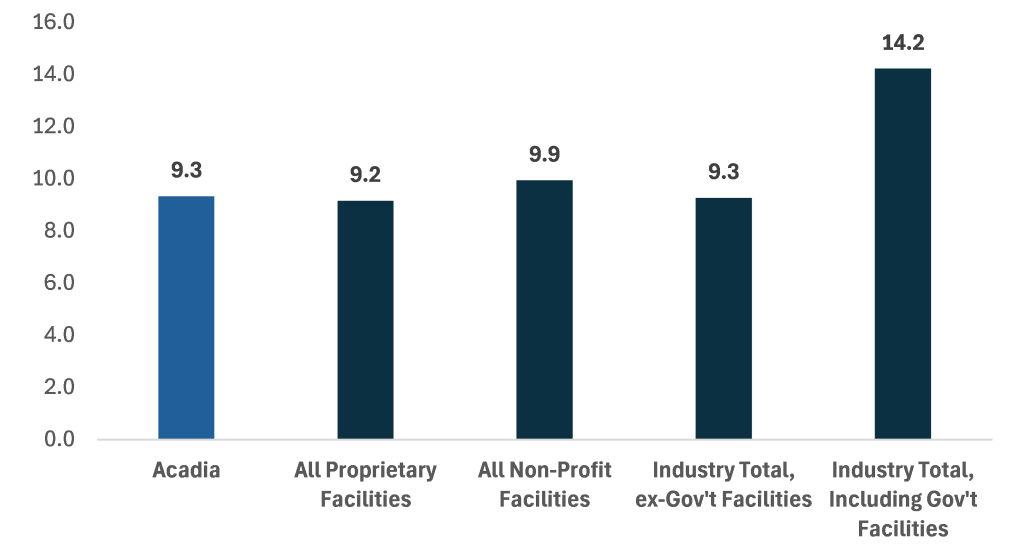
*Healthcare cost reporting information system (HCRIS) from CMS
Patient care decisions, including whether treatment is necessary and for how long, are medical decisions made by licensed providers, based on medical necessity and adhere to all associated legal requirements.
In addition, multi-disciplinary teams work with patients, guardians, and family members during their treatment and in preparation for discharge. Discharging a patient too early can result in catastrophic consequences, including serious injury – and even death – for the patient or others. When making discharge decisions, physicians lead with the best interests of our patients and weigh a variety of factors including ongoing treatment needs and the risk of discharging before adequate stabilization.
Acadia is proud of the support we provide to those requiring acute psychiatric care
In 2023, 81% of our patients who responded to a survey – including involuntarily admitted respondents – reported feeling hopeful as a result of the care they received in our hospitals. And since 2016, Acadia has provided over $500 million in uncompensated care to help deliver the best outcomes for patients regardless of ability to pay. We remain steadfast in our commitment to ensuring patients, families, and their communities have access to the highly specialized treatment delivered at our hospitals.
Acadia hospitals are highly regulated, independently accredited and uphold stringent standards
Our hospitals are highly regulated and are required to meet policies and standards set by federal, state, and local governments. All 54 of Acadia’s acute hospitals are licensed in each state, accredited by TJC and overseen by independent, respected third party organizations and government entities such as CMS. This oversight helps ensure compliance with policies governing reimbursement and care quality, including from all government healthcare programs.
These independent bodies regularly visit – unannounced – to evaluate our compliance and ensure we provide high quality, effective care for our patients. Acadia’s acute care hospitals have been inspected nearly 300 times per year on average over the past five years. In addition, we are routinely subjected to other federal, state and local inspections as well as independent audits by third-party firms. We also regularly welcome third parties into our hospitals on a daily basis – from case managers to payors and other independent healthcare professionals – to review patient progress and collaborate in discharge planning.
Certain media reports lack important facts and context about involuntary commitment cases
Involuntary commitment to a psychiatric hospital is a complex issue with profound implications for individuals and their families. While some stories have portrayed commitment as a means of trapping individuals against their will, the process is far more complicated. In most cases, the decision to involuntarily commit a patient for psychiatric evaluation in a behavioral health hospital is initiated by emergency room providers, law enforcement personnel, or other individuals designated by state statutes. Those independent third parties make the initial determination that a patient requires an urgent psychiatric assessment. Once admitted, a psychiatric evaluation is then conducted to determine a treatment or discharge plan.
It is important to emphasize that involuntary commitment includes a legal process that generally involves many parties, such as a patient attorney, family members, the court system, case managers, law enforcement and outside referring clinicians.
We understand the tremendous responsibility that comes with supporting patients admitted involuntarily to our hospitals. These are serious decisions, and our clinicians fiercely advocate for our patients’ best interests.
Inaccurate portrayals of Acadia hospitals in the media perpetuate harmful beliefs about behavioral healthcare
Inaccurate and incomplete reporting about behavioral healthcare may unfortunately reinforce the fear and misconceptions some may have about seeking treatment. These reports may even perpetuate the myth that psychiatric care is ineffective or even harmful.
As part of our commitment to deliver technology-driven quality care, Acadia continues to invest millions of dollars annually into our hospitals. We also partner with many of the most highly respected, well-established health systems throughout the country to expand access to life saving behavioral health care in local communities. Additionally, it is important to acknowledge the dedication of our 23,500 Acadia employees who come to work every day living our purpose to Lead Care with Light in support of patients, families and communities seeking hope for brighter futures.
Acadia remains focused on addressing our country’s mental health crisis
Our country is facing a severe mental health crisis. According to Mental Health America, over half of adults with a mental illness receive no treatment. Given our nation’s record level of suicide rates, it is critical to ensure patients needing behavioral healthcare can receive proper treatment.
Acadia is committed to improving access to care and making the system easier to navigate for patients. We remain focused on providing the supportive, collaborative and compassionate care that is so desperately needed.
